Concerned parents typically fill the daily appointment schedule of a paediatic health care clinician with common complaints such as:
“Her school report says she can’t keep up with her classmates and she always complains about participating in P.E”
“The school nurse called again today and he has had another fall and knocked out both front teeth”
“Every day it’s a different spot that she points to, she says it’s so painful”
“I can’t take him shopping with me as he needs me to pick him up all the time, he’s just too heavy for me to carry now”
Some of these complaints can sound like a typically developing child with an over concerned parent. Sometimes there is something more sinister at play.
When exploring pain and gross motor concerns in children, your clinical assessment for this type presentation should also result in a list of differential diagnoses. Joint hypermobility should be high on that list, along with developmental coordination disorders, concerns with vision or vestibular function, poor muscle strength and endurance or types of connective tissue disorders.
In typically developing children, there often can be some degree of hypermobility that doesn’t cause pain, motor delay or reduced participation in activity(1). But Benign Joint Hypermobility Syndrome (BJHS) can account for over 25% of all referrals to Paediatric Rheumatoloty clinics(3).
The Beighton scale is a type of assessment that has established validity and reliability in the assessment of hypermobility in children(4). This scale forms a key part of the diagnostic criteria medical professionals will use for formal diagnosis when all other heritable disorders of connective tissue have been excluded (1,5). However BJHS and Ehlers-Danlos Syndrome hypermobile types are consider clinically indistinguishable(6)
Instructions during the performance of the Beighton scale(7):
- I am going to bend your little finder up at 90° degrees to the back of your hand
- I am going to bend your thumb back on the front of your forearm
- I am going to bend your elbow backward
- I am going to bend your knee backward
- Can you put your hands flat on the floor with your knees straight
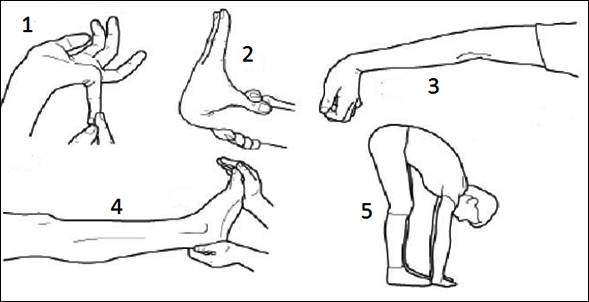
Scoring the Beighton Scale(7)
| LEFT | RIGHT | |
| 1. Passive dorsiflexion and hyperextension of the fifth joint beyond 90° | 1 | 1 |
| 2. Passive apposition of the thumb to the flexor aspect of the forearm | 1 | 1 |
| 3. Passive hyperextension of the elbow beyond 10° | 1 | 1 |
| 3. Passive hyperextension of the knee beyond 10° | 1 | 1 |
| 5. Active forward flexion of the trunk with knee fully extended so that the palms of the hand are flat on the floor | 1 | 1 |
| TOTAL | /9 | |
Symptoms of BJHS include:
- Chronic pain in multiple joints(8)
- Recurrent joint dislocation, headaches and general chest pain(8)
- Gastrointestinal involvement such as; stress incontinence, abdominal pain, dizziness(8)
- Skin involvement such as; stretch marks, poor scar heeling and soft skin(8)
- Physiological effects such as depression and anxiety (8)
Pain levels and reduced balance in children with BJHS appears to have a large effect on activity levels(9). The most painful joints being the feet and knees(2), which are significantly increased in the presence of obesity (9). The consequence is an “at risk health related quality of life” that clusters these children with those suffering from chronic conditions such as cancer, obesity, hypoplasia of the left ventricle and fibromyalgia(10). This greatly highlights the disabling nature of joint hypermobility on children. Pacey et al (2015) found that there appeared to be a cascade of problems seen with children with BJHS. Children would have no symptoms, and then experience an injury or insidious intractable pain that lead to deconditioning and/or weight gain, this could then result in exacerbation of symptoms and reduced health related quality of life.
The British Society for Paediatric and Adolescent Rheumatology in 2013 (11) released guidelines for the management of BJHS in children and young people. Their recommendation was that general hypermobility should be regarded as a connective tissue advantage providing the child was strong and fit. Difficulties occurred mainly when the body became weak and deconditioned. Treatment should be centered on self-management, technique and pain management to:
Build and maintain muscle strength and function
Restore effective and efficient movement patterns
Improve fitness
Restore normal range of movement
Improve proprioception
The treatment of a child with BJHS should be undertaken within a multidisciplinary approach including medical and allied health clinicians. If you would like further details please visit: http://www.arthritisvic.org.au
References (A selection of these articles are available within the members only references area):
1. Jull-Kristensen B, Kristensen JH, Frausing B, Jensen DV, Rogind H, Remig L. Motor competence and physical activity in 8 year old school children with generallised joint hypermobility. Pediatrics 2009; 124(50: 1380-1387
2. Schubert-Hjalmarsson E, Ohman A, Kyllerman M; Pain, Balance, Activity and Participation in children with hypermobility syndrome. Journal of Pediatric Physical Therapy 2012; 24:339-334
3. Kerr A, Macmillan CE, Uttley WS, Luqmani RA. Physiotherapy for children with hypermobility syndrome. Physiotheapy 2000 86: 313-17
4. VerDerGiessen L, Liekens D, Reutgers K, Hartmen A, Mulder P, Oranje A. Validation of Beighton Score and prevalence in connective tissue signs in 773 dutch children. J Rheumatology 2001; 28(12) 2726-2730
5. Grahame R, Bird HA, Child A. The revised criteria for the diagnosis of benign joint hypermobility syndrome. Journal of Rheumatology 2000; 27: 1777-9
6. Tinkle BT, Bird HA, Grahame R The lack of clinical distinction between the hypermobility type of Ehleers-Danlos syndrome and the joint hypermobility syndrome AM j Med Genet A 2009; 149A 2368-70
7. Alter M. Science of Flexibility. Sheridan books 2004 (third edition); page 89
8. Smith T, Easton V, Bacon H, Jerman E, Armon K, Poland F, Macgregor A The relationship between benign joint hypermobility syndrome and psychological distress: a systematic review and meta analysis. Rheumatology 2013
9. Pacey V, Tofts L, Adams R, Munns C, Nicholson L. Joint hypermobility syndrome subclassification in paediatrics: a factor analytic approach. Arch Dis Child (2015); 100: 8-13
10. Pacey V, Tofts L, Adams R, Munns C, Nicholson L. Quality of life prediction in children with joint hypermobilty syndrome. Journal of paediatrics and child health 51 (2015) 689-695
11. The British Society for Paediatric and Adolescent Rheumatology. Guidelines for the management of joint hypermobility syndrome in children and young people. (2013)
