By: Simone Cranage
Bow legs is a common complaint seen by podiatrist. It is often when a child begins to stand and walk, that the appearance of their legs triggers parental concern.
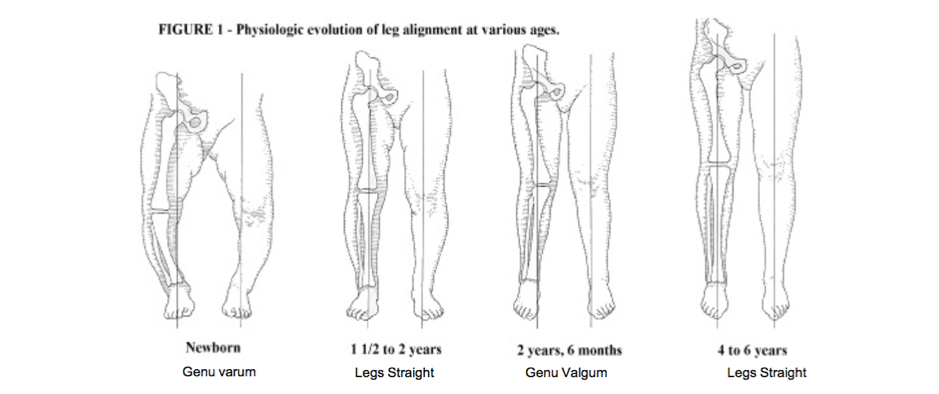
Legs goes through a number of alignment progressions as a child grows from varus (bow legs) to valgus (knock knees) and there is a wide range of normal values within this range. At birth, normal alignment is in varus, with maximal bow legs at the age of 6 months.
The alignment becomes more neutral or straight between the ages of 18 months to 2 years, before progressing to a valgus alignment, with the greatest amount of “knock-kneedness” observed at 4 years of age [1].
After the age of 4, this alignment generally decreases towards adult alignment of slight valgus (knock kneed) to neutral (straight) alignment (Figure 1- Source unknown).
It is increasingly important that we are confident in our assessment of a child presenting with genu varum so that we can differentiate a normal physiological alignment from a potential pathological cause.
The majority of children with bowed legs will have physiologic bowing, which presents as bilateral and symmetrical in nature.
The natural history of physiologic bowing is spontaneous correction and the The Victorian Paediatric Orthopaedic Network have developed a great evidence based parent handout which explain the natural progression from bow legs to knock knees.
Most young children with bow legs have physiologic varus, however it is important for us as clinicans to recognise those children that are falling outside of normal ranges. So there are a number of key examinations and red flags highlighting when intervention is needed?
Earlier detection of a child with pathological bow leg deformity will hopefully have improved outcomes overall for a child. A thorough history taking is one of the most important parts of our assessment.
History taking: The following questions are important to consider when a child presents with bow legs.
- Growth and development of the child- how are they tracking for their height, weight and BMI for their age?
- Onset of the bowing- was this prior to or after walking?
- Progression of the deformity- has the severity increased with time?
- Are there any associated complaints such as falling, limping, tripping or in-toeing?
- Is there a family history of anything similar in appearance or short stature?
- Has the child had any previous treatment and how did they respond to this?
- What is the child’s dietary and vitamin intake (specifically calcium and Vitamin D)
- Do they have enough sunlight exposure?
- Is there any history of infection, trauma or a fracture?
Assessment: Following our history taking, there may be additional triggers for further testing in particular the following:
- Height and weight percentiles
- Assessment in-toeing
- Measurement of inter-condylar distance in standing with feet together (or supine if not yet standing)
- Assessment of leg length discrepancy- shortening of the legs may be an indication of skeletal dysplasia or asymmetrical physeal growth
- Gait assessment- observation of a lateral thrust (lateral knee joint protrusion during stance phase)
Following our assessment, if there is any identified deviation from normal, as clinicians we should be thinking about an appropriate referral for the child presenting to us. There may be consideration of an orthopaedic surgeon, endocrinologist or geneticist based on clinical findings. There are a number of resources that exist which can assist in decision making on whether a referral is appropriate. The Victorian Paediatric Orthopaedic Network has developed guidelines for referral into a specialist clinic, which includes the following criteria:
Red Flags:
- Persistence of bow legs after 3 years
- Intercondylar separation >6cm (distance between the femoral condyles)
- Asymmetrical deformity
- Excessive deformity
- Progressive deformity or lack of resolution
- Pain
- Following a traumatic event
- Height below 5th centile for age (other associated skeletal deformity- skeletal dysplasia, Ricket’s)
An understanding of normal physiological bowing is essential in differentiating physiologic from pathologic alignment. It is also important to have possible differential diagnoses in mind while assessing a child presenting with bow legs. Pathological causes of bow legs generally do not spontaneous resolve and further assessment and treatment is required. At the end of the day, if you are unsure and if there are any red flags to indicate the presenting complaint may not be physiologic in nature, a referral would be recommended. It is important to consider, there is no podiatry interventions that have any evidence of impacting on bowed legs. Our role is identification of pathology and most importantly, reassurance when the presentation is a typical variation.
Pathological causes of bow legs include:
- Blount’s disease (Obesity is a risk factor for adolescent Blount’s disease)
- Nutritional rickets and other metabolic bone diseases
- Skeletal dysplasia
- Infection
- Trauma
- Neoplasia
These conditions will be covered further in future blogs.
Reference:
1. Heath, C.H. and L.T. Staheli, Normal limits of knee angle in white children--genu varum and genu valgum. J Pediatr Orthop, 1993. 13(2): p. 259-62.
